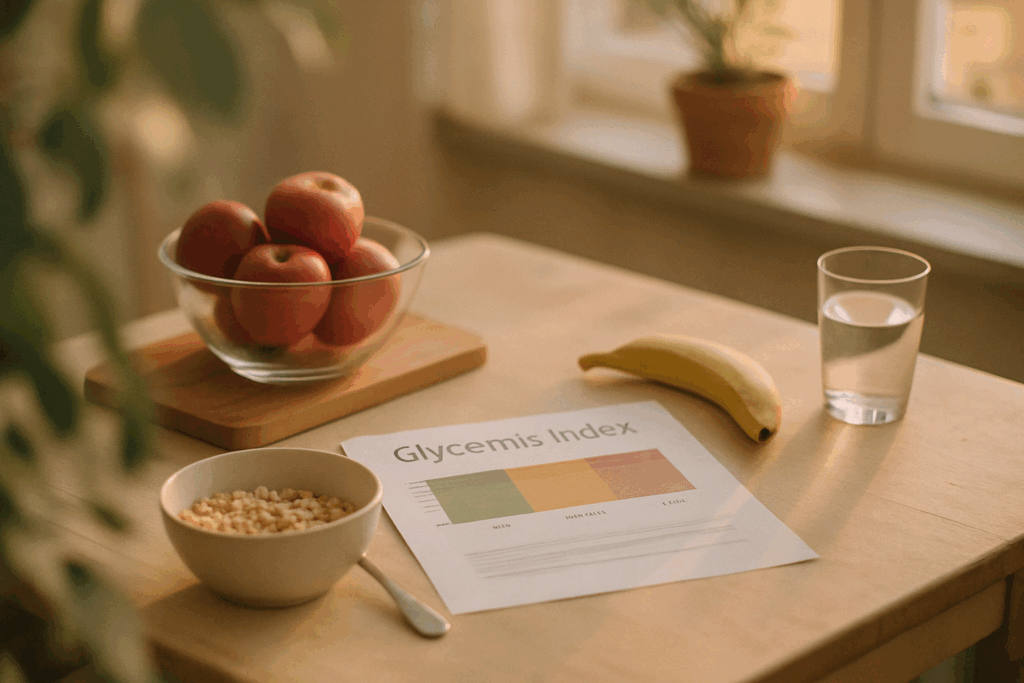
What the Glycemic Index Really Measures
The glycemic index (GI) is a way of ranking carbohydrates based on how quickly they raise blood sugar after eating. It’s not about carbs being good or bad it’s about how fast your body breaks them down and turns them into glucose. The faster that happens, the higher the GI.
The ranking uses a scale from 0 to 100, with pure glucose pegged at 100. Foods are tested based on their ability to spike blood sugar compared to this baseline. The higher the number, the quicker the spike.
Here’s the basic breakdown:
Low GI (≤55): These are the slow burners things like lentils, sweet potatoes, and most non starchy vegetables. They digest gradually, giving you more stable energy.
Medium GI (56 69): These are in the middle examples include brown rice and whole wheat bread. Not too fast, not too slow.
High GI (≥70): These hit your bloodstream fast. Think white bread, instant rice, and sugary cereals.
Bottom line: The GI gives a clear picture of how carbs behave in your body. It’s a useful starting point for making smarter food choices especially if your goal is better energy levels, fewer crashes, or managing blood sugar.
Why the GI Matters in 2026
The glycemic index (GI) isn’t just a nutrition buzzword it’s a simple way to understand how food affects your blood sugar. High GI foods (think white bread, sugary snacks, or instant cereals) cause rapid spikes in blood glucose. Low GI items, like legumes or steel cut oats, digest more slowly, resulting in steadier energy and less strain on your system.
Why does that matter? Constant blood sugar spikes can wear down insulin sensitivity over time. When your body has to pump out more insulin to keep glucose levels stable, it starts to lose its edge. That’s a fast track to fatigue, cravings, and eventually, insulin resistance.
For people managing prediabetes, type 2 diabetes, or metabolic syndrome, this link is critical. Choosing lower GI foods can help improve glucose control, support more consistent energy throughout the day, and ease the burden on the pancreas. In a world of desk jobs and 24/7 snacking, the GI can be a reliable anchor in the chaos.
Glycemic Index vs. Glycemic Load
The glycemic index (GI) tells you how fast a food spikes your blood sugar, but it leaves out one major variable: how much of that food you’re actually eating. That’s where glycemic load (GL) steps in.
Glycemic load accounts for both the quality (GI) and the quantity (carbohydrate content per serving) of the food. In simple terms, it gives you a more realistic look at how a typical portion size will impact your blood sugar.
Take watermelon. It has a high GI up around 72 but a low GL. Why? Because watermelon is mostly water and relatively low in carbs per serving. So unless you’re eating a truckload, it won’t slam your blood sugar the way, say, a slice of white bread will. That same piece of white bread has both a high GI and a high GL. The result: quick spike, fast crash.
For people watching their blood sugar whether for energy, weight, or metabolic health using both GI and GL together is the smart move. Think of GI as speed and GL as the size of the fuel tank. Fast doesn’t matter as much if there’s hardly any fuel. But fast with a full tank? That’s a blood sugar rollercoaster. Know both. Use both.
The goal isn’t just slow carbs, but smart carbs. And knowing the difference helps you eat better without overthinking every bite.
Common High vs. Low GI Foods
Not all carbs hit your bloodstream the same way. High glycemic index (GI) foods like white bread, instant rice, and sugary breakfast cereals are digested fast. They hit your system like a sugar bomb, spiking blood sugar and insulin quickly. Good for quick fuel, not great for long term stability.
On the other end, you’ve got the slow burners. Think lentils, steel cut oats, and non starchy vegetables like broccoli or spinach. These sit at the low end of the GI scale. They take longer to break down, which means steadier energy and fewer blood sugar swings.
But here’s the twist: how you prepare your food changes its GI. Cook pasta too long, and the GI shoots up. Mash your potatoes smooth, and you’re looking at a faster digesting carb. The more processed or overcooked a food is, the more likely it’ll rank high. So it’s not just what you eat it’s how you prep it that counts.
Practical Tips for Stabilizing Blood Sugar
Eating for stable blood sugar isn’t about cutting out every high GI food it’s about balance. A slice of white bread on its own might spike your glucose, but pair it with avocado or eggs, and the fat and protein slow that spike down. Same with fruit: have a banana with a spoonful of peanut butter or a handful of nuts, and you’ve got a better situation on your hands.
The key is combining high GI foods with fiber, protein, or healthy fats. These nutrients blunt blood sugar surges and help your body burn through the carbs more gradually. Think grilled chicken with sweet potatoes and sautéed greens not just a giant bowl of plain pasta.
Balanced meals beat the numbers game. Low GI doesn’t always mean healthy, and high GI doesn’t always mean harmful. Context is everything. If your meal has some starch, make sure it’s surrounded by stuff that keeps your metabolism grounded.
For snacks, go for combos that hold you over without crashing you like hummus and raw veggies, Greek yogurt with berries, or apple slices and almond butter. Avoid the grab and go granola bars with sugar as the first ingredient. Smoother energy comes from smarter pairing, not just eating less.
Bottom line: don’t stress the GI too hard. Use it as a signal, not a rule. Your body runs best on variety, balance, and foods that work together.
The GI and Anti Inflammatory Eating Patterns
Low GI foods don’t just keep your blood sugar in check they also help dial down systemic inflammation. That matters, because chronic inflammation is linked to everything from heart disease and diabetes to depression. When you eat foods that release glucose slowly, you avoid the metabolic firestorms that high GI meals can trigger.
Whole foods like legumes, berries, leafy greens, and intact whole grains not only rate low on the glycemic index they’re also loaded with antioxidants, phytonutrients, and fiber. This combo helps your immune system stay sharp without tipping into overdrive. Processed carbs and added sugars, on the other hand, tend to spike blood glucose fast, which kicks off a chain reaction: insulin rushes in, inflammatory markers go up, and energy crashes follow.
So if your goal is steady energy, better immunity, and long term health, the low GI route makes sense. Focus on meals built around whole, minimally processed ingredients. This isn’t about obsessing over numbers it’s about giving your body foods that work with it, not against it.
For a deeper look at the relationship between food and inflammation, check out What You Need to Know About Anti Inflammatory Diets.
Final Notes on Using the GI Wisely
The glycemic index (GI) is useful but it’s not gospel. It wasn’t designed to dictate every food choice or demonize your favorite fruit. Instead, it’s a tool to help you think more critically about how different foods affect your blood sugar. The problem starts when people use it in a vacuum, obsessing over numbers instead of patterns.
Diet isn’t a single meal or snack. It’s everything you eat, day after day. That means individual GI values make more sense when you consider the full picture: what you’re eating it with, how much you’re eating, your activity level, and your metabolism. A high GI food paired with fat and protein won’t hit your system the same way as it would on its own.
Stay grounded. Whole foods, balanced meals, and consistency matter far more than hitting some magic GI target. Mix your carbs with fiber, use hydration and movement to your advantage, and don’t sweat the small stuff. Long term health is built on patterns, not perfection.